 There are two different types of veins inside the leg. There are superficial veins, which sit just below the skin and are easily seen on the surface. These often are the ones that develop varicosities or spider veins. Then there are deep veins which are located deep within the muscles of the legs. Blood flows between the superficial veins and the deep veins through smaller veins, called perforator veins. Both superficial and perforator veins have one-way valves that allow the blood to flow in only one direction.
There are two different types of veins inside the leg. There are superficial veins, which sit just below the skin and are easily seen on the surface. These often are the ones that develop varicosities or spider veins. Then there are deep veins which are located deep within the muscles of the legs. Blood flows between the superficial veins and the deep veins through smaller veins, called perforator veins. Both superficial and perforator veins have one-way valves that allow the blood to flow in only one direction.
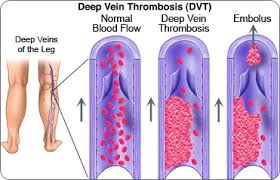
Blood clots can form in either the superficial veins or the deep veins. When they form in the superficial veins there is very little risk that they will travel and cause problems in other areas of the body. They form, for the most part, along a track of vein that has become varicose because of the stagnation of the blood. The same is true for blood clots that form in the deep vein systems. They form because of the stagnation, the inability of the blood to move quickly, through the venous system.
A person has an increased risk of a clot forming in their deep veins when they travel for long distances in a car, train or plane. All of these involve prolonged sitting with knees bent at 90°. Individuals who are hospitalized and are not up and moving around also have an increased risk as well is individuals who have undergone surgery. Any time there is a trauma to the lower leg, whether there is surgery or a cast placed or not, the individual has an increased risk of developing a deep vein thrombosis.
Other risk factors include pregnancy, obesity, certain types of medications such as birth control pills, smoking, genetic predisposition, cancer, fracture to the leg or a complication of an invasive procedure done to a vein. (1) Individuals who have varicose veins have been found to be at higher risk for the development of deep vein thrombosis. (2)
The blood clot within the deep vein is not dangerous in itself. However, it becomes life-threatening when a piece of the clot breaks off and travels through the venous system, back to the heart and into the pulmonary system. It is at this point it can become lodged in the lungs and cause a pulmonary embolism. This pulmonary embolism will cut off blood supply to specific portions of the lungs and can result in death.
Treatment for deep vein thrombosis can take several different paths. For the most part, physicians will recommend the use of medications, including use of anticoagulant, to decrease the possibility that more clots will form or the original clot will become larger. These medications decrease the ability of the blood to clot and can cause other issues if the individual is injured in any way. Initial treatment will be done using heparin injections in the hospital and then the patient will take a pill after being discharged for several months. (3,4)
 It is important that you take your anticoagulant medication exactly as instructed. These medications have serious side effects when there is too much taken or not enough. The absorption of these medications can also be affected by an individual’s nutritional intake and periodic blood tests are required in order to monitor the situation.
It is important that you take your anticoagulant medication exactly as instructed. These medications have serious side effects when there is too much taken or not enough. The absorption of these medications can also be affected by an individual’s nutritional intake and periodic blood tests are required in order to monitor the situation.
If anticoagulants aren’t successful, or if the physician feels you have a more serious type of deep veins, other medications may be tried. Thrombolytics are drugs given through an intravenous line and used to break up clots. They are usually called tissue plasmogen activators (TPA) and commonly used in individuals who present to the hospital in the initial stages of a heart attack or stroke in order to break up those clots. These drugs can cause serious bleeding and are typically used only in life-threatening situations.
If you have any other underlying medical conditions which do not allow you to take in anticoagulant medication, blood thinner, then a filter may be inserted into a large vein in your lower abdomen. This filter prevents any clot that breaks loose from lodging in your lungs, which is ultimately the most serious side effect of a deep vein thrombosis. The filters are sometimes referred to as the umbrellas because of the way that they look and the function they provide.
Your physician may also recommend the use of compression stockings to help prevent swelling. The pressure helps to reduce the chance that the blood will continue to clot and cause more deep vein or superficial vein thrombosis. Individuals who have been diagnosed with the deep vein thrombosis should wear their compression stockings for at least one year if possible.
In a pilot study released in 2008, researchers from the National Institutes of Health in Bethesda, Maryland found that injections of fiber-binding thrombolytic agent around the clot will effectively treat the area and reduce the risk of a recurrence. The treatment appears to clear the clots and restore blood flow quickly. (5)
If the deep vein thrombosis occurred in the upper leg, above the knee, the individual will probably need to take an anticoagulant therapy for up to six months or longer. After six months the physician may recommend you continue anticoagulant therapy to prevent any more clots from recurring, depending upon your overall medical condition.
As with most medical conditions it is easier to prevent than it is to treat. Minimize your risk factors by participating in regular exercises, reducing the amount of time you are sitting or standing for long lengths of time, reducing your overall weight and pressure placed on your lower extremities, and make wise lifestyle choices, such as quitting smoking or reducing your on-call intake. When hospitalized for any reason request compression stockings or balloon stockings to continue to assist your lower extremities to return blood to the heart. Be sure to get out of bed, as possible, and walk through the hospital several times each day.
References:
(1) Centers for Disease Control and Prevention: Are You At Risk for deep Vein Thrombosis?
www.cdc.gov/Features/Thrombosis
(2) American Academy of Orthopaedic Surgeons: Untreated Varicose Veins Increase DVT Risk in THA Patients
www.aaos.org/news/acadnews/2012/AAOS11_2_8.asp
(3) Journal of the American Society of Hematology: How We Diagnose and Treat Deep Vein Thrombosis
www.bloodjournal.hematologylibrary.org/content/99/9/3102.long
(4) American Family Physician: DVT and Pulmonary Embolism: Part II Treatment and Prevention
www.aafp.org/afp/2004/0615/p2841.html
(5) Radiologic Society of North America: New Therapy Effectively Treats Deep Vein Thrombosis
www.sciencedaily.com/releases/2008/01/080129080704.htm


Leave a Reply