 Graves’ disease is an autoimmune condition in which the body attacks the thyroid gland resulting in an overproduction of thyroid hormones (thyrotoxicosis). The condition is named after Robert Graves, a 19th-century Irish physician who discovered and described the condition. Graves’ disease can have an effect on many different parts of the body such as the nervous system, eyes, skin, hair and nails, lungs, digestive system and reproductive system. This broad number of bodily systems affected by Graves’ disease points to the complex nature of the human body.
Graves’ disease is an autoimmune condition in which the body attacks the thyroid gland resulting in an overproduction of thyroid hormones (thyrotoxicosis). The condition is named after Robert Graves, a 19th-century Irish physician who discovered and described the condition. Graves’ disease can have an effect on many different parts of the body such as the nervous system, eyes, skin, hair and nails, lungs, digestive system and reproductive system. This broad number of bodily systems affected by Graves’ disease points to the complex nature of the human body.
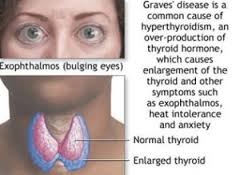
In Graves’ disease the thyroid gland in the neck is enlarged and hyperactive, producing excessive amounts of thyroid hormone. Graves’ disease is eight times more common in women than men and most frequently occurs between the age of 20 and 40. It does have a familial tendency, which means that it runs in families. The disease is characterized by a formation of autoantibodies that bind to receptors in the thyroid membrane and stimulate the gland.
Symptoms of Graves’ disease will be similar to hyperthyroidism, a condition that can be caused by Graves’ disease. Classic symptoms include an enlarged gland, nervousness, heat intolerance, weight loss, sweating, diarrhea, tremors, palpitations and exophthalmus (a swelling of the tissue behind the eyes which causes the protrusion of the eyeball).
A complication of the disease can lead to a life-threatening heart, liver and kidney failure. This is called a thyroid storm which can begin suddenly and caused by a stressful event. The signs and symptoms include extreme irritability, high blood pressure, rapid heart rate, vomiting, high fever, delirium and coma. Left untreated, this thyroid storm will be fatal.
If Graves’ disease is left untreated it can cause severe thyrotoxicosis. Cardiac complications and psycho-cognitive complications will cause significant morbidity. Hyperthyroidism will increase muscle energy expenditure and muscle protein breakdown. These abnormalities can explain the sarcopenia and myopathy observed in patients who have hyperthyroid Graves’ disease. Cardiac hypertrophy (enlargement of the heart muscle) is also reported in individuals who experienced thyrotoxicosis. Rhythm disturbances such as atrial fibrillation and flutter are also common.
Individuals will suffer from psychiatric manifestations from an over production of thyroid hormone, such as mood and anxiety disorders. Progression of ophthalmoopathy can lead to compromised vision and blindness. Pregnant women can transfer thyroid stimulating antibodies to their neonate causing hyperthyroidism in the baby.
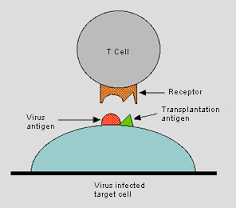 Researchers believe that Graves’ disease may be a result of an expression of a viral antigen in the body which triggers the immune system to attack the thyroid gland. There may also be an alteration of T cell antibodies and is influenced by a combination of environmental and genetic factors. Environmental factors associated with susceptibility are largely unproven at this point. Smoking has been implicated in worsening of vision in individuals who have Graves’ disease.
Researchers believe that Graves’ disease may be a result of an expression of a viral antigen in the body which triggers the immune system to attack the thyroid gland. There may also be an alteration of T cell antibodies and is influenced by a combination of environmental and genetic factors. Environmental factors associated with susceptibility are largely unproven at this point. Smoking has been implicated in worsening of vision in individuals who have Graves’ disease.
Graves’ disease can be diagnosed from the results of one or two simple tests. However, your physician may use several methods to double check the findings and rule out any other underlying medical conditions which may mimic Graves’ disease. An analysis of the blood should show levels of two hormones which are produced or regulated by the thyroid. These levels will be higher than normal if an individual suffers from Graves’ disease.
Treatment for Graves’ disease addresses the symptomatology and not the underlying cause. There is no current treatment to stop the immune system from producing antibodies and so medications and drugs are used to control the signs and symptoms designed to decrease the production of thyroxine or to block its action. Beta-blockers are medications used to relieve hyperthyroid symptoms such as rapid heart rate, nervousness and tremors. The body continues to produce too much thyroid hormone but the beta-blockers will block some of the action of the hormone and are often used in conjunction with other forms of treatment.
Anti-thyroid medications include Tapazole, which will prevent the thyroid from producing excessive amounts of hormone. Treatment typically goes on for a year and sometimes two which will cause a long-term remission of the disease. However, relapse is increasingly common. These drugs are often used with radioactive iodine treatment or surgery to help control the signs and symptoms of the disease.
To make the thyroid hormone the body uses iodine. If an individual takes in radioactive iodine this is collected in the thyroid gland that over time the radioactivity destroys the overactive cells. This causes the thyroid gland to shrink and the problems will lessen gradually, usually over several weeks or several months. Because the treatment causes death in the thyroid cells, individuals will require a thyroid hormone replacement at the end of treatment.
However, radioactive iodine treatment can increase the risk for visual effects which can be mild and temporary but may not be recommended if you already have moderate to severe eye problems.
If an individual cannot tolerate anti-thyroid medications and does not want use radioactive iodine therapy then, the third option is surgery to remove the thyroid gland. After surgery thyroid replacement hormone will be necessary to supply the body with the normal amounts of hormones needed to function appropriately. Risks of this surgery include potential damage to the vocal cords and parathyroid glands. The parathyroid glands will produce a hormone that controls the level of calcium in the blood and is necessary to maintain optimal health.
Individuals who suffer from the effects to their eyes from Graves’ disease will also require other medications, orbital decompression surgery, eye muscle surgery or a specific type of glasses in order to control double vision. Any of these types of treatment protocols will be evaluated based on the individuals overall health, and severity of their disease.
Resources:
Graves’ Disease and Thyroid Foundation: Living with Graves’ Disease
http://www.gdatf.org/about/about-graves-disease/living-with-graves-disease/
National Endocrine and Metabolic Diseases Information Service: Graves’ Disease
http://www.endocrine.niddk.nih.gov/pubs/graves/
MedlinePlus: Graves’ Disease
http://www.nlm.nih.gov/medlineplus/ency/article/000358.htm
Women’s Health.gov: Graves’ Disease Fact Sheet
http://womenshealth.gov/publications/our-publications/fact-sheet/graves-disease.cfm


Leave a Reply